Endocrine
Meerensee Medical Centre
Advanced Medicine
Hypothyroidism - Hashimoto's
Hashimoto‘s hypothyroidism, also known as Hashimoto’s thyroiditis, is an autoimmune disorder in which the immune system attacks the thyroid gland, leading to inflammation and eventual destruction of thyroid tissue. This condition primarily affects women and typically develops between the ages of 30 and 50, although it can occur at any age.
Symptoms of Hashimoto’s hypothyroidism include:
- Fatigue: Patients often experience excessive tiredness and a lack of energy, even after getting enough sleep.
- Weight gain: Unexplained weight gain, despite no change in diet or exercise habits, is a common symptom.
- Cold intolerance: Individuals with Hashimoto’s hypothyroidism may feel cold more easily than others, even in warm environments.
- Constipation: Sluggish bowel movements and difficulty passing stool are common complaints.
- Dry skin and hair: Skin may become dry, flaky, and prone to itching, while hair may become brittle and thin.
- Muscle weakness and joint pain: Weakness in the muscles, especially in the arms and legs, and joint pain are frequently reported symptoms.
- Depression and mood changes: Hashimoto’s hypothyroidism can lead to mood swings, irritability, and depression.
- Menstrual irregularities: Women may experience heavy or irregular menstrual periods, or even amenorrhea (absence of menstruation).
- Bradycardia: A slower than normal heart rate may occur, leading to feelings of fatigue and dizziness.
- Swelling of the thyroid gland (goiter): In some cases, the thyroid gland may become enlarged, causing visible swelling in the neck.
Hashimoto’s hypothyroidism can be diagnosed through blood tests that measure levels of thyroid-stimulating hormone (TSH) and thyroxine (T4). Treatment typically involves thyroid hormone replacement therapy to supplement the body’s low thyroid hormone levels and alleviate symptoms. Regular monitoring and adjustments to medication dosage may be necessary to ensure optimal thyroid function and symptom management.
Graves Disease
Symptoms of Graves’ disease include:
- Hyperactivity and restlessness: Patients may experience increased energy levels, nervousness, and difficulty relaxing or sleeping.
- Weight loss: Despite having an increased appetite, individuals with Graves’ disease often lose weight unintentionally.
- Rapid heartbeat (tachycardia): A fast or irregular heartbeat, palpitations, and sensations of a pounding heart are common.
- Heat intolerance: Patients may feel excessively warm or sweat more than usual, even in cooler environments.
- Tremors and muscle weakness: Fine tremors, particularly in the hands, and muscle weakness are frequently reported symptoms.
- Fatigue and weakness: Despite increased energy levels, individuals may experience muscle weakness and fatigue due to the strain on the body.
- Frequent bowel movements: Diarrhea or more frequent bowel movements than usual may occur.
- Changes in menstrual patterns: Women may experience irregular menstrual periods or amenorrhea (absence of menstruation).
- Exophthalmos (bulging eyes): Graves’ disease can cause the eyes to protrude from their sockets, leading to a characteristic bulging appearance.
- Thyroid enlargement (goiter): The thyroid gland may become visibly enlarged, causing swelling in the neck.
Diagnosis of Graves’ disease involves blood tests to measure levels of thyroid hormones (T4 and triiodothyronine [T3]) and thyroid-stimulating hormone (TSH). Additionally, imaging studies such as ultrasound or radioactive iodine uptake tests may be performed to assess thyroid function and evaluate the presence of a goiter.
Treatment options for Graves’ disease include medications to block the production of thyroid hormones (such as antithyroid drugs like methimazole or propylthiouracil), radioactive iodine therapy to destroy thyroid tissue, or surgical removal of part or all of the thyroid gland (thyroidectomy). Each treatment approach has its own risks and benefits, and the choice of treatment depends on factors such as the patient’s age, overall health, and preferences. Additionally, supportive measures to manage symptoms, such as beta-blockers to control heart rate and manage tremors, may be recommended. Regular monitoring of thyroid function is essential to ensure proper management of Graves’ disease and prevent complications.
Polycystic Ovarian Syndrome
Polycystic ovary syndrome (PCOS) is a hormonal disorder that affects women of reproductive age, often presenting with a range of symptoms related to hormonal imbalances. The exact cause of PCOS is not fully understood, but it involves a combination of genetic and environmental factors.
Symptoms of PCOS include:
Irregular menstrual periods: Women with PCOS often have irregular menstrual cycles, with intervals longer than 35 days or fewer than eight menstrual cycles per year. Some may also experience heavy or prolonged menstrual bleeding.
Ovulatory dysfunction: PCOS can cause anovulation, where the ovaries do not release eggs regularly, leading to fertility issues and difficulty conceiving.
Hyperandrogenism: Elevated levels of androgens (male hormones) such as testosterone may lead to symptoms such as:
- Excess facial and body hair growth (hirsutism), particularly on the face, chest, back, and abdomen.
- Acne: PCOS-related hormonal imbalances can contribute to acne outbreaks, particularly on the face, chest, and upper back.
- Male-pattern baldness or thinning hair (alopecia): Some women with PCOS may experience hair loss or thinning of the hair on the scalp, similar to male-pattern baldness.
Polycystic ovaries: On ultrasound examination, the ovaries may appear enlarged and contain multiple small follicles, giving them a characteristic appearance described as “polycystic.”
Insulin resistance and metabolic abnormalities: Many women with PCOS have insulin resistance, which can lead to elevated insulin levels and an increased risk of developing type 2 diabetes. Other metabolic abnormalities associated with PCOS include obesity, dyslipidemia (abnormal lipid levels), and hypertension (high blood pressure).
Weight gain: PCOS is often associated with weight gain or difficulty losing weight, particularly around the abdomen.
Skin changes: Darkening of the skin, particularly in body creases such as the neck, groin, and underneath the breasts (acanthosis nigricans), may occur in some women with PCOS, especially those who are insulin resistant.
Diagnosis of PCOS involves a thorough medical history, physical examination, and laboratory tests to assess hormone levels, including testosterone, luteinizing hormone (LH), follicle-stimulating hormone (FSH), and fasting glucose and insulin levels. Imaging studies such as ultrasound may also be performed to evaluate the ovaries.
Management of PCOS focuses on addressing individual symptoms and underlying hormonal imbalances. Treatment options may include lifestyle modifications (such as weight loss, dietary changes, and regular exercise) to improve insulin sensitivity, medications to regulate menstrual cycles (such as hormonal contraceptives or ovulation-inducing drugs), and treatments to manage symptoms such as hirsutism and acne (such as anti-androgen medications or topical therapies). Additionally, fertility treatments may be recommended for women trying to conceive. Long-term management of PCOS aims to reduce the risk of complications such as diabetes, cardiovascular disease, and endometrial cancer through regular monitoring and appropriate interventions.

Endometriosis
Endometriosis is a chronic and often painful condition in which tissue similar to the lining of the uterus (endometrium) grows outside the uterus, commonly on the ovaries, fallopian tubes, outer surface of the uterus, and other pelvic organs. This misplaced tissue responds to hormonal changes in the menstrual cycle, thickening, breaking down, and bleeding with each menstrual cycle, but unlike the normal endometrium shed during menstruation, the blood and tissue shed by endometrial implants have no way to exit the body. This can lead to inflammation, scarring, and the formation of adhesions, causing pain, infertility, and other complications.
Symptoms of endometriosis include:
Pelvic pain: Chronic pelvic pain that may worsen during menstruation, intercourse, or bowel movements is a hallmark symptom of endometriosis. The severity of pain can vary from mild to severe.
Dysmenorrhea: Painful menstrual periods (dysmenorrhea) characterized by pelvic cramping and lower abdominal pain are common in women with endometriosis.
Painful intercourse (dyspareunia): Pain during or after sexual intercourse is frequently reported by women with endometriosis.
Painful bowel movements or urination: Endometrial implants on the bowel or bladder can cause pain during bowel movements or urination, particularly during menstruation.
Heavy menstrual bleeding: Some women with endometriosis may experience heavy menstrual bleeding (menorrhagia) or irregular bleeding between periods.
Infertility: Endometriosis can affect fertility by causing inflammation, scarring, and obstruction of the fallopian tubes, impairing egg release, and disrupting implantation.
Fatigue and low energy: Chronic pain and associated symptoms of endometriosis can lead to fatigue and a decreased quality of life.
Estrogen Dominance
Estrogen dominance is a hormonal imbalance characterized by high levels of estrogen relative to progesterone in the body. Estrogen dominance can contribute to the development and exacerbation of endometriosis by promoting the growth of endometrial tissue and inflammation in the body.
Symptoms of estrogen dominance may include:
Irregular menstrual cycles: Estrogen dominance can cause changes in menstrual patterns, such as irregular or heavy periods.
Breast tenderness: Swollen or tender breasts, particularly before menstruation, may occur in women with estrogen dominance.
Mood swings: Fluctuations in estrogen levels can affect mood and emotional well-being, leading to mood swings, irritability, or anxiety.
Weight gain: Estrogen dominance may contribute to weight gain, particularly in the hips, thighs, and abdomen.
Fibrocystic breasts: Estrogen dominance can lead to the development of fibrocystic breast changes, characterized by lumps, swelling, or pain in the breasts.
Headaches: Some women with estrogen dominance may experience headaches or migraines, particularly around menstruation.
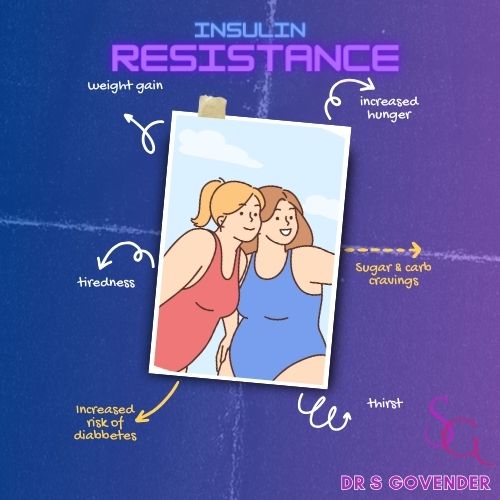
Insulin Resistance
Insulin resistance is a metabolic condition in which the body’s cells become less responsive to the effects of insulin, a hormone produced by the pancreas that helps regulate blood sugar levels. When cells become resistant to insulin, they are less able to efficiently take up glucose from the bloodstream, leading to elevated blood sugar levels (hyperglycemia). To compensate for this resistance, the pancreas produces more insulin, resulting in higher-than-normal insulin levels in the blood (hyperinsulinemia).
Insulin resistance is a key feature of type 2 diabetes, but it can also occur in individuals without diabetes and is often associated with other metabolic conditions, such as obesity, metabolic syndrome, and polycystic ovary syndrome (PCOS).
Symptoms of insulin resistance may include:
Elevated blood sugar levels: Insulin resistance can lead to persistently high levels of glucose in the bloodstream, especially after meals.
Fatigue and low energy: Despite high blood sugar levels, cells may not receive an adequate supply of glucose for energy production, leading to fatigue and feelings of lethargy.
Increased hunger and cravings: Insulin resistance can disrupt the body’s ability to regulate appetite and satiety, leading to increased hunger and cravings, especially for sugary or high-carbohydrate foods.
Weight gain: Insulin resistance is closely linked to obesity and abdominal fat accumulation, which further exacerbates insulin resistance and increases the risk of developing type 2 diabetes and other metabolic conditions.
Difficulty losing weight: Insulin resistance can make it challenging to lose weight, even with diet and exercise, due to impaired glucose metabolism and increased fat storage.
Darkened skin patches: Some individuals with insulin resistance may develop acanthosis nigricans, characterized by dark, velvety patches of skin, typically in body creases such as the neck, armpits, or groin.
Polycystic ovary syndrome (PCOS): Insulin resistance is a common feature of PCOS, contributing to hormonal imbalances and symptoms such as irregular menstrual periods, hirsutism (excess facial and body hair), and infertility.
High blood pressure: Insulin resistance is associated with hypertension (high blood pressure), which increases the risk of cardiovascular disease and other complications.
Diagnosis of insulin resistance typically involves blood tests to measure fasting blood sugar levels, insulin levels, and sometimes other markers such as hemoglobin A1c (HbA1c) or glucose tolerance tests. Treatment and management of insulin resistance focus on improving insulin sensitivity and controlling blood sugar levels through lifestyle modifications (such as diet, exercise, and weight management) and medications (such as insulin sensitizers or glucose-lowering drugs). Additionally, managing associated conditions such as obesity, hypertension, and dyslipidemia (abnormal lipid levels) is essential for reducing the risk of cardiovascular disease and other complications associated with insulin resistance.
Fatty Liver
Fatty liver disease, also known as hepatic steatosis, is a condition characterized by the accumulation of fat in the liver cells. This excess fat can interfere with liver function and lead to inflammation, scarring (fibrosis), and potentially progress to more severe liver diseases such as non-alcoholic fatty liver disease (NAFLD) or non-alcoholic steatohepatitis (NASH). Fatty liver disease can be classified into two main types:
Non-alcoholic fatty liver disease (NAFLD): This is the most common form of fatty liver disease and is not related to excessive alcohol consumption. NAFLD encompasses a spectrum of conditions ranging from simple fatty liver (steatosis) to non-alcoholic steatohepatitis (NASH), which involves liver inflammation and damage. NAFLD is closely associated with obesity, insulin resistance, type 2 diabetes, high cholesterol, and metabolic syndrome.
Alcoholic fatty liver disease: This type of fatty liver disease is caused by excessive alcohol consumption over time. Alcohol is metabolized by the liver, and chronic alcohol abuse can lead to the accumulation of fat in liver cells, inflammation, and liver damage. Alcoholic fatty liver disease can progress to more severe liver conditions such as alcoholic hepatitis and cirrhosis if alcohol consumption continues.
Symptoms of fatty liver disease may include:
Fatigue and weakness: Many individuals with fatty liver disease experience fatigue and a decreased energy level, which can affect daily activities.
Abdominal discomfort: Some people may experience discomfort or pain in the upper right abdomen, where the liver is located.
Enlarged liver: In some cases, the liver may become enlarged and tender to the touch.
Elevated liver enzymes: Blood tests may reveal elevated levels of liver enzymes such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST), indicating liver inflammation or damage.
Jaundice: In more advanced cases of liver disease, jaundice may occur, causing yellowing of the skin and eyes.
Ascites: Fluid buildup in the abdominal cavity (ascites) may occur in severe cases of liver disease, leading to abdominal swelling and discomfort.
Diagnosis of fatty liver disease typically involves a combination of medical history, physical examination, blood tests (including liver function tests and tests to assess for other potential causes of liver disease), imaging studies such as ultrasound, CT scan, or MRI, and sometimes liver biopsy to assess the degree of liver damage and inflammation.
Treatment of fatty liver disease focuses on addressing underlying risk factors and lifestyle modifications to reduce fat accumulation in the liver and prevent disease progression. This may include:
- Weight loss: Achieving and maintaining a healthy weight through diet and exercise is key to reducing liver fat and improving insulin sensitivity.
- Diet modification: Following a balanced diet low in saturated fats, refined carbohydrates, and added sugars can help improve liver health.
- Regular exercise: Engaging in regular physical activity can help reduce liver fat, improve insulin sensitivity, and promote overall health.
- Management of underlying conditions: Treating conditions such as obesity, diabetes, high cholesterol, and metabolic syndrome can help improve liver function and reduce the risk of complications.
- Avoidance of alcohol: For individuals with alcoholic fatty liver disease, avoiding alcohol consumption is essential to prevent further liver damage.
- Medications: In some cases, medications may be prescribed to manage underlying conditions or to target specific aspects of liver disease, such as insulin resistance or inflammation.
- Close monitoring: Regular follow-up with healthcare providers and monitoring of liver function is important to assess disease progression and response to treatment.


Fatty Liver - Impending Doom
Fatty liver disease, once considered a minor health concern, has now emerged as a significant public health issue worldwide. As a doctor, it’s crucial to educate patients about the potential dangers of fatty liver and its implications for overall health. In this article, we’ll delve into why fatty liver is more than just a benign condition and explore its potential consequences if left untreated.
What is Fatty Liver? Fatty liver, medically known as hepatic steatosis, occurs when excess fat accumulates in the liver cells. While it’s normal for the liver to contain some fat, when more than 5-10% of the liver’s weight is fat, it’s considered fatty liver disease. This condition is commonly associated with excessive alcohol consumption (alcoholic fatty liver disease) or non-alcoholic factors such as obesity, insulin resistance, high blood sugar, and high levels of fats in the blood.
Why is Fatty Liver Bad for Your Health?
Liver Inflammation: Fatty liver can lead to inflammation of the liver, a condition known as steatohepatitis. This inflammation can cause liver cells to become damaged and scarred, leading to a more severe form of liver disease called non-alcoholic steatohepatitis (NASH). NASH increases the risk of developing complications such as liver cirrhosis and liver cancer.
Liver Cirrhosis: Prolonged inflammation and liver cell damage can progress to cirrhosis, a late stage of scarring (fibrosis) of the liver. In cirrhosis, healthy liver tissue is replaced by scar tissue, impairing liver function. Cirrhosis can lead to complications such as fluid buildup in the abdomen (ascites), bleeding disorders, liver failure, and an increased risk of liver cancer.
Increased Risk of Cardiovascular Disease: Fatty liver is closely linked to metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes. People with fatty liver often have elevated levels of triglycerides and LDL cholesterol, as well as insulin resistance, which can contribute to atherosclerosis (hardening and narrowing of the arteries) and cardiovascular complications.
Risk of Liver Cancer: While not everyone with fatty liver disease will develop liver cancer, studies have shown that people with NASH-related cirrhosis are at an increased risk of developing liver cancer (hepatocellular carcinoma). Liver cancer is often diagnosed at an advanced stage, making it difficult to treat and reducing the chances of survival.
Impact on Overall Health: Beyond its direct effects on the liver, fatty liver disease can have systemic consequences that affect overall health. It is associated with an increased risk of other chronic conditions such as kidney disease, sleep apnea, and certain types of cancer.
Conclusion: Fatty liver disease is far from a benign condition and can have serious implications for your health if left untreated. As a doctor, it’s essential to raise awareness about the potential dangers of fatty liver and encourage patients to adopt a healthy lifestyle that includes regular exercise, a balanced diet, maintaining a healthy weight, and avoiding excessive alcohol consumption. Early detection and intervention are key to preventing the progression of fatty liver disease and reducing the risk of complications. By prioritizing liver health, we can safeguard overall well-being and longevity.

Menopausal High Androgens
High androgens in menopause, particularly in women experiencing symptoms of hyperandrogenism, can be indicative of several conditions. Androgens are male hormones that are also present in smaller amounts in females. During menopause, hormonal fluctuations can lead to changes in androgen levels, and some women may experience an increase in androgen production or sensitivity, which can contribute to various symptoms.
Common symptoms of high androgens in menopause may include:
- Hirsutism: Excessive hair growth in areas typically associated with male-pattern hair growth, such as the face (upper lip, chin), chest, back, and abdomen.
- Acne: Increased androgen levels can stimulate sebum production in the skin, leading to acne outbreaks, particularly along the jawline, chin, and lower face.
- Male-pattern baldness: Thinning of the hair on the scalp, similar to male-pattern baldness, may occur in women with high androgen levels.
- Irregular menstrual cycles: Menopause itself is characterized by the cessation of menstrual periods, but irregular bleeding or spotting may occur due to hormonal fluctuations, including high androgen levels.
- Mood changes: Androgens can influence mood and emotional well-being, and some women may experience mood swings, irritability, or symptoms of depression or anxiety.
- Decreased libido: Changes in androgen levels can affect sexual desire and libido in menopausal women.
- Weight gain: High androgen levels may contribute to abdominal weight gain and difficulty losing weight.
- Insulin resistance: Elevated androgen levels can be associated with insulin resistance, which may increase the risk of developing type 2 diabetes and metabolic syndrome.
- Polycystic ovary syndrome (PCOS): Some menopausal women may have undiagnosed or pre-existing PCOS, a condition characterized by high androgen levels, irregular menstrual cycles, and ovarian cysts.
It’s essential for menopausal women experiencing symptoms of hyperandrogenism to undergo a thorough evaluation by a healthcare provider to determine the underlying cause and appropriate management. This may involve a combination of medical history, physical examination, blood tests (including hormone levels such as testosterone and other androgens), imaging studies (such as ultrasound), and possibly other diagnostic tests.
Treatment of high androgens in menopause depends on the underlying cause and may include:
- Hormone replacement therapy (HRT): In some cases, hormone therapy with estrogen and/or progestin may help regulate hormone levels and alleviate symptoms of menopause, including those related to high androgens.
- Anti-androgen medications: Medications that block the effects of androgens or reduce their production may be prescribed to manage symptoms such as hirsutism, acne, and hair loss.
- Lifestyle modifications: Healthy lifestyle habits, including regular exercise, a balanced diet, stress management, and adequate sleep, can help support hormonal balance and overall well-being.
- Topical treatments: For symptoms such as acne or hirsutism, topical treatments such as retinoids or anti-androgen creams may be recommended.
- Management of underlying conditions: Treating underlying conditions such as PCOS, insulin resistance, or metabolic syndrome may help improve androgen levels and alleviate symptoms.
- Close monitoring: Regular follow-up with healthcare providers is important to monitor symptoms, hormone levels, and response to treatment, and to adjust treatment as needed.
Low Testosterone levels in Men
Low testosterone levels in men, also known as hypogonadism or testosterone deficiency, can occur due to various factors, including aging, medical conditions, lifestyle factors, and certain medications. Testosterone is a crucial hormone in men responsible for regulating various bodily functions, including sexual development, libido, muscle mass, bone density, mood, and energy levels. When testosterone levels drop below normal, it can lead to a range of symptoms.
Common symptoms of low testosterone levels in men may include:
- Decreased libido: One of the hallmark symptoms of low testosterone is a reduced interest in sex or a decline in sexual desire.
- Erectile dysfunction: Low testosterone can contribute to difficulties achieving or maintaining erections during sexual activity.
- Fatigue and low energy: Men with low testosterone levels may experience fatigue, decreased energy levels, and a lack of motivation.
- Decreased muscle mass and strength: Testosterone plays a role in building and maintaining muscle mass, so low levels can lead to reduced muscle strength and size.
- Increased body fat: Low testosterone levels may contribute to an increase in body fat, particularly around the abdomen.
- Mood changes: Testosterone influences mood, and low levels can lead to feelings of depression, irritability, or decreased overall well-being.
- Decreased bone density: Testosterone helps maintain bone density and strength, so low levels may increase the risk of osteoporosis and fractures.
- Hair loss: Some men with low testosterone levels may experience thinning of the hair or loss of body and facial hair.
- Difficulty concentrating: Testosterone plays a role in cognitive function, and low levels may contribute to difficulties with memory, concentration, and mental clarity.
- Decreased sperm production: Testosterone is essential for sperm production, so low levels may affect fertility and sperm quality.
Diagnosis of low testosterone levels in men involves a combination of medical history, physical examination, and blood tests to measure testosterone levels. It’s important for healthcare providers to rule out other potential causes of symptoms and to assess for any underlying medical conditions that may be contributing to low testosterone levels.
Treatment options for low testosterone levels in men may include:
- Testosterone replacement therapy (TRT): TRT involves the administration of testosterone through various methods, such as injections, patches, gels, or implants, to restore testosterone levels to normal range.
- Lifestyle modifications: Making lifestyle changes such as regular exercise, maintaining a healthy weight, getting enough sleep, and reducing stress can help support testosterone production and overall health.
- Treatment of underlying conditions: Addressing underlying medical conditions such as obesity, diabetes, or thyroid disorders may help improve testosterone levels.
- Medication adjustments: In some cases, medications that may be contributing to low testosterone levels, such as certain antidepressants or corticosteroids, may be adjusted or discontinued.
- Close monitoring: Regular follow-up with healthcare providers is important to monitor testosterone levels, symptoms, and response to treatment, and to make any necessary adjustments to the treatment plan.

Hormonal Hair Loss
Hormonal hair loss, also known as androgenetic alopecia or pattern hair loss, is a common condition characterized by gradual thinning of the hair, typically on the scalp, due to hormonal factors. It is the most common cause of hair loss in both men and women and is influenced by genetic predisposition and hormonal fluctuations, particularly involving androgens (male hormones) such as testosterone and its derivative, dihydrotestosterone (DHT).
In individuals predisposed to hormonal hair loss, hair follicles become sensitive to the effects of DHT, which leads to a shortening of the hair growth cycle and miniaturization of the hair follicles. Over time, affected hair follicles produce finer, shorter hairs, eventually leading to visible thinning of the scalp hair.
Hormonal hair loss typically follows a specific pattern, which differs between men and women:
In men:
- Male-pattern baldness typically begins with hair thinning at the temples and crown, resulting in a receding hairline and a characteristic “M” shape. Over time, hair loss may progress to more extensive balding on the top of the scalp, leaving a horseshoe-shaped pattern of hair around the sides and back of the head.
In women:
- Female-pattern hair loss tends to be more diffuse, with gradual thinning of the hair on the crown of the scalp. Women may notice widening of the part line and decreased hair density, but they typically retain their frontal hairline.
While hormonal hair loss is influenced by genetic predisposition and hormonal factors, other factors such as age, stress, medical conditions, medications, and environmental factors may also play a role in exacerbating or accelerating hair loss.
Treatment options for hormonal hair loss may include:
Medications:
- Minoxidil (Rogaine): A topical medication applied to the scalp, minoxidil can help promote hair regrowth and slow down hair loss in both men and women with androgenetic alopecia.
- Finasteride (Propecia): This oral medication works by blocking the conversion of testosterone to DHT, thereby reducing the levels of DHT in the scalp and slowing down hair loss in men with male-pattern baldness. It is not typically recommended for use in women due to potential side effects.
Low-level laser therapy (LLLT): LLLT devices, such as laser combs or helmets, deliver low-energy laser light to the scalp, which is believed to stimulate hair follicles and promote hair regrowth.
Platelet-rich plasma (PRP) therapy: PRP involves injecting a concentrated solution of the patient’s own platelets into the scalp to stimulate hair growth and improve hair density.
Hair transplantation: Surgical procedures such as follicular unit transplantation (FUT) or follicular unit extraction (FUE) can be used to transplant hair follicles from areas of the scalp resistant to hair loss (donor area) to areas of thinning or baldness (recipient area).
Lifestyle modifications: Adopting a healthy lifestyle, managing stress, and avoiding harsh hair treatments or styling practices can help support overall hair health and minimize hair loss.
It’s important for individuals experiencing hormonal hair loss to consult with a healthcare provider or dermatologist to determine the underlying cause of hair loss and develop a personalized treatment plan tailored to their specific needs and preferences.
Hormonal Hair Loss Management
Objective:
Please note that this protocol is designed for our patients with hormonal hair loss, we have assessed and identified the reason for their hair loss. They are being treated accordingly. There are numerous causes for hair loss. Please speak to your doctor to assess you and create a custom plan for you.
Consistency and patience is your key to success, as visible results may take several months to appear.
1. Shampoo
Recommendation: A shampoo with a DHT-blocker.
- Usage:
- Frequency: 2 times a week.
- Instructions: Leave the shampoo on the scalp for 5 – 10 minutes before rinsing to allow for maximum absorption of active ingredients.
2. Microneedling
Recommendation: Use a dermaroller with 0.5mm to 1.5mm needle length.
- Frequency: Once a week.
- Instructions:
- Preparation: Ensure the scalp is clean and dry. Disinfect the dermaroller with isopropyl alcohol.
- Procedure: Roll the dermaroller over the affected areas of the scalp in vertical, horizontal, and diagonal directions. Apply gentle pressure to avoid injury.
- Post-Care: Clean the dermaroller with alcohol after each use. Avoid washing the scalp for at least 24 hours post-treatment.
3. Topical Hair Loss Formulation
Recommendation: Minoxidil based solution or a custom compounded formula. This is ordered on an individual basis.
- Frequency: Twice daily.
- Instructions:
- Application: Apply the recommended amount (usually 1 mL) directly to the affected areas of the scalp.
- Technique: Part the hair to ensure the solution reaches the scalp. Rub in gently with fingertips.
- Post-Application: Do not rinse the product out. Allow it to dry naturally.
4. Oral Supplementation
Recommendation: A combination of vitamins, minerals, and supplements that support hair health and address hormonal imbalances.
Monitoring and Follow-up
- Initial Assessment: Conduct a thorough medical history and scalp examination to determine the cause of hair loss and rule out any underlying conditions.
- Regular Check-ups: Schedule follow-up appointments every 3-6 months to monitor progress, assess treatment efficacy, and adjust the protocol as needed.
- Blood Tests: Periodically check blood levels of relevant hormones, vitamins, and minerals to ensure they are within optimal ranges.
Lifestyle and Dietary Recommendations
- Diet: Encourage a balanced diet rich in protein, healthy fats, and antioxidants. Include foods such as eggs, nuts, seeds, fish, and leafy green vegetables.
- Hydration: Advise drinking plenty of water to maintain scalp and hair health.
- Stress Management: Recommend stress reduction techniques such as yoga, meditation, or regular exercise.
Hormonal Acne
Hormonal acne is a type of acne that is primarily influenced by hormonal fluctuations in the body, particularly fluctuations in androgen levels. Androgens are male hormones that are present in both men and women, and they play a role in stimulating the production of sebum (oil) in the skin’s oil glands. When sebum production increases, it can lead to clogged pores and the growth of acne-causing bacteria, resulting in the development of acne lesions.
Hormonal acne typically occurs during periods of hormonal changes, such as puberty, menstruation, pregnancy, and menopause. It is more common in women than men, and it often presents as deep, cystic lesions, particularly along the jawline, chin, and lower face. Hormonal acne may also be associated with other symptoms of hormonal imbalances, such as irregular menstrual cycles, hirsutism (excessive hair growth), and scalp hair thinning.
Common characteristics of hormonal acne include:
Deep, cystic lesions: Hormonal acne often presents as large, inflamed pimples or cysts beneath the surface of the skin. These lesions can be painful and may take longer to heal compared to other types of acne.
Pattern of occurrence: Hormonal acne tends to occur in specific areas of the face, particularly along the jawline, chin, and lower face. It may also appear on the neck, chest, and back.
Fluctuating severity: Hormonal acne may fluctuate in severity over time, often worsening before menstruation (premenstrual acne) and improving during other phases of the menstrual cycle.
Persistence: Hormonal acne may persist into adulthood, particularly in women with underlying hormonal imbalances or conditions such as polycystic ovary syndrome (PCOS).
Treatment options for hormonal acne may include:
Topical treatments: Over-the-counter or prescription topical treatments containing ingredients such as benzoyl peroxide, salicylic acid, retinoids (such as adapalene or tretinoin), or azelaic acid can help reduce inflammation, unclog pores, and promote skin cell turnover.
Oral medications: In cases of severe or persistent hormonal acne, oral medications such as oral contraceptives (birth control pills), spironolactone (an anti-androgen medication), or oral antibiotics (such as doxycycline or minocycline) may be prescribed to regulate hormone levels, reduce sebum production, and control acne-causing bacteria.
Hormonal therapy: For women with underlying hormonal imbalances or conditions such as PCOS, hormonal therapy may be recommended to regulate menstrual cycles and hormone levels, which can help improve acne symptoms.
Lifestyle modifications: Adopting a healthy lifestyle, including regular exercise, a balanced diet, stress management, and proper skincare habits, can help support overall skin health and reduce the severity of hormonal acne.
Professional treatments: Procedures such as chemical peels, microdermabrasion, or laser therapy may be recommended by dermatologists to help improve acne lesions and promote clearer skin.
It’s important for individuals with hormonal acne to consult with a dermatologist or healthcare provider to determine the underlying cause of their acne and develop a personalized treatment plan tailored to their specific needs and skin type. With proper treatment and management, hormonal acne can be effectively controlled, and the appearance of the skin can be improved.
Cushing Syndrome
Cushing syndrome occurs due to prolonged exposure to high levels of the hormone cortisol. Here are the main causes:
Exogenous (external) corticosteroids: This is the most common cause. Long-term use of corticosteroid medications, such as prednisone, prescribed for conditions like asthma, arthritis, or autoimmune diseases, can lead to Cushing syndrome.
Pituitary adenoma (Cushing’s disease): A benign tumor of the pituitary gland causes overproduction of adrenocorticotropic hormone (ACTH), which stimulates the adrenal glands to release excess cortisol.
Ectopic ACTH production: Some tumors outside the pituitary gland, like lung cancer, can produce ACTH, leading to high cortisol levels.
Adrenal tumors: Tumors in the adrenal glands (benign or malignant) can independently produce excess cortisol.
Familial Cushing syndrome: In rare cases, genetic mutations may predispose individuals to develop tumors that cause Cushing syndrome.
These causes result in a range of symptoms like weight gain, high blood pressure, osteoporosis, and changes in mood or energy levels.