Blog
Meerensee Medical Centre
Advanced Medicine
Symptoms
- Feeling hungry even after a meal
- Sugar and Carb Cravings
- Tiredness
- Struggling to lose weight
- Puts on weight easily post diet/ exercise vacation
- Abdominal Fat
- Recurrent Infections
How to Manage?
Improve Insulin Sensitivity
- Speak to your doctor about assessment and medication
- High Fiber Diet
- Exercise
- Loss of body fat
Understanding Estrogen Dominance
Symptoms
- Loss of Lean Muscle Mass
- Moodiness
- Depression
- Water Retention
- Belly Fat
- Chest Fat/ Gynaecomastia “man Boobs” (Men)
- Difficulty losing weight
- Tiredness
- Poor erection (men)
- Low Libido
How to Manage?
- Speak to your doctor about assessment and medication.
- High Fiber Diet, Green Vegetables, Fruits especially Citrus Fruits
- Lean Meat, High Protein Diet
- Exercise
- Loss of body fat
- Avoid Alcohol and Limit Caffeine
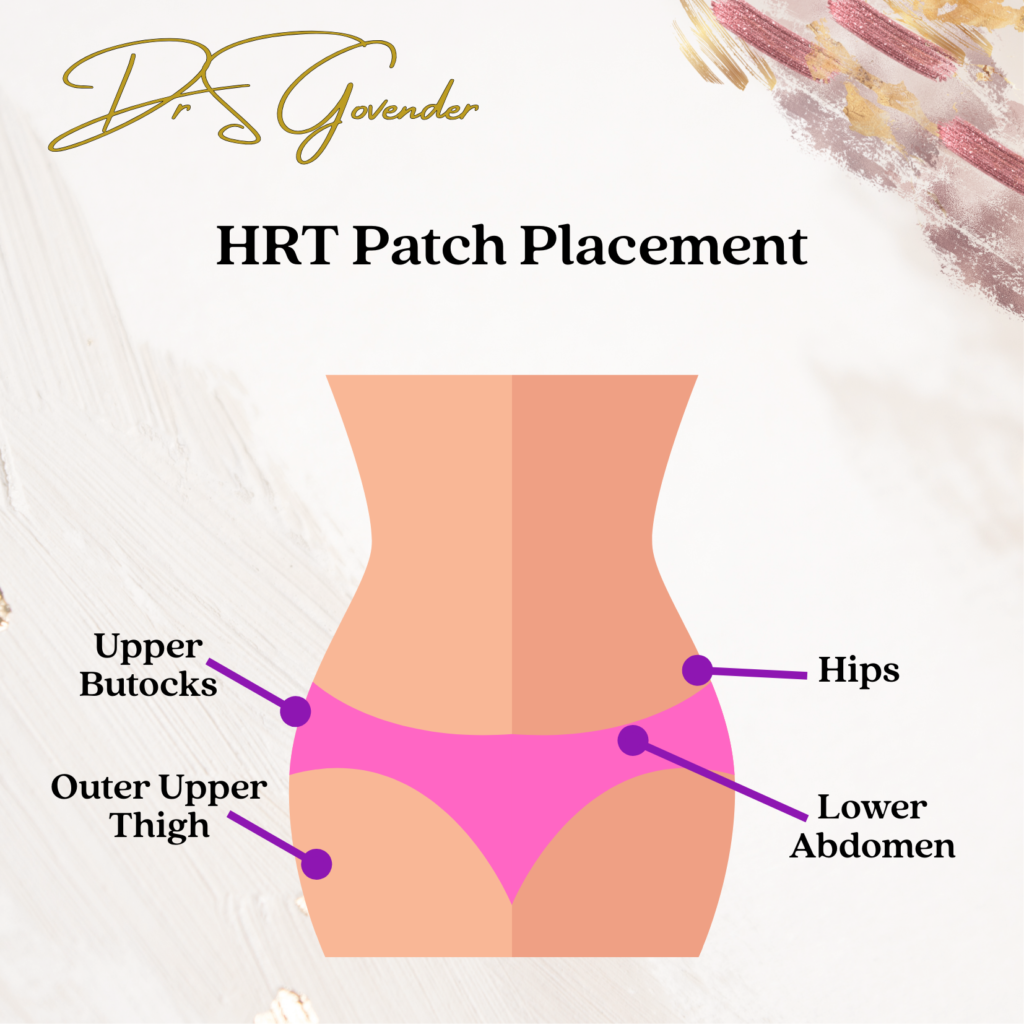
HRT Patches
Using Utrogestan

Metabolic Disease and Kidney Stones
The link between metabolic syndrome, diabetes and kidney stones. Each of these conditions is interrelated in various ways, particularly through shared risk factors like obesity, insulin resistance, and poor dietary habits.
The following ways are how they are linked:
1. Metabolic Syndrome and Kidney Stones
- Metabolic syndrome is a cluster of conditions including obesity, high blood pressure, high blood sugar, abnormal cholesterol levels, and insulin resistance. These factors increase the risk of developing kidney stones.
- Insulin resistance (a hallmark of metabolic syndrome) can affect the kidneys’ ability to handle calcium, oxalate, and uric acid, leading to the formation of kidney stones.
- People with metabolic syndrome often have low urine pH, which increases the risk of forming uric acid stones.
2. Diabetes and Kidney Stones
- Type 2 diabetes, particularly when poorly controlled, is linked to a higher risk of kidney stones. Diabetics often have more acidic urine, which can promote the formation of uric acid stones.
- Insulin resistance in diabetes may alter kidney function and reduce the ability of the kidneys to properly excrete waste products like oxalate, which can contribute to kidney stone formation.
- Diabetics may also experience dehydration due to higher blood glucose levels, which increases the concentration of stone-forming substances in the urine.
3. Common Pathways and Risk Factors
- Obesity: A key component of both metabolic syndrome and diabetes, obesity is a significant risk factor for kidney stones. Excess weight increases the amount of waste the kidneys filter, leading to more stone-forming compounds in the urine.
- Diet: High sugar, high salt, and high-fat diets, often linked to metabolic syndrome and diabetes, can also increase the risk of kidney stones.
- Insulin resistance: This condition impacts how the body processes substances like calcium and oxalate, which can lead to a higher risk of kidney stones in both metabolic syndrome and diabetes.
4. Increased Uric Acid Levels
- Both metabolic syndrome and diabetes are associated with higher levels of uric acid in the blood, which can lead to uric acid stone formation in the kidneys.
In summary, metabolic syndrome, diabetes, and kidney stones are connected by common risk factors such as insulin resistance, obesity, and dietary habits. Managing metabolic health can help reduce the risk of developing kidney stones, especially for those with diabetes.
Vaginosis
Definition
Vaginosis is an inflammation of the vagina caused by a shift in the normal flora balance (good bacteria in the vagina). There are 2 types: Bacterial Vaginosis and a Vaginal Yeast Infection.
- Bacterial Vaginosis is an overgrowth of bad bacteria.
- Vaginal Yeast Infection is an overgrowth of yeast that causes irritation, discharge and intense itchiness of the vagina and vulva.
Causes
It is not a sexually transmitted infection. It can be caused by Perfumed Bubble Bath, Soap, Shower gel, Strong detergent used to was underwear, a Douche or Vaginal Deodorant.
Treatment
Use a Gentle Washing Agent
- Bioderma Face Wash
- Cerave Face Wash
- Eucerine Body Wash
Treat Bacterial Overgrowth with Vaginal Gel.
Treat Yeast Overgrowth with Anti-Fungal Cream.
Use a zinc oxide cream to heal and help with vaginal pain and discomfort.
Perimenopause is a natural phase of life, but it can come with a mix of confusing, frustrating, and sometimes surprising changes. If you’re in your 40s (or even late 30s) and starting to feel “off” in a way that’s hard to explain, this might be why.
In this post, we’ll walk you through what perimenopause actually is, the most common and lesser-known symptoms, and how to take care of yourself during this time—without getting lost in medical jargon.
What is Perimenopause?
Perimenopause is the transitional stage before menopause. During this time, your hormone levels—especially oestrogen and progesterone—start to fluctuate. Your menstrual cycle may become irregular, and a variety of physical and emotional symptoms can start to appear.
This phase can last several years. It ends when you’ve gone 12 consecutive months without a period, which is when menopause officially begins.
When Does Perimenopause Start?
Most women begin perimenopause in their 40s, but for some, it may start earlier. The experience can be different from one person to the next—some go through it gradually, while others notice changes almost overnight.
Common Perimenopause Symptoms
You might experience:
Hot flushes and night sweats
Irregular periods (heavier, lighter, longer, or more spaced out)
Mood swings, irritability or anxiety
Trouble sleeping or waking up feeling unrefreshed
Fatigue, even after a full night’s sleep
Vaginal dryness or discomfort
Changes in libido
These symptoms can vary in intensity and may come and go.
Lesser-Known Symptoms You Might Not Expect
Perimenopause can also bring some unexpected symptoms:
Brain fog – forgetfulness or trouble concentrating
Palpitations – a fluttering or racing heartbeat
Joint pain or muscle stiffness
Tingling in the hands or feet
Worsening of PMS
Increased headaches or migraines
Weight gain, especially around the middle
These are all valid and recognised effects of hormonal fluctuations. You’re not imagining things.
What Causes These Changes?
The main drivers are shifting hormone levels—especially oestrogen and progesterone. These hormones don’t decline in a steady line. Instead, they rise and fall unpredictably, which is why symptoms can feel so inconsistent.
Your body is adapting, and while the process is entirely natural, it can still feel disruptive.
Taking Care of Yourself During Perimenopause
There are many ways to manage perimenopause and support your wellbeing. These small, sustainable lifestyle changes can make a big difference:
Move Your Body
Gentle and consistent movement helps with mood, sleep, joint pain and weight. Walking, swimming, yoga or strength training are all great options.
Eat to Nourish
Focus on whole foods, leafy greens, fibre, calcium-rich options, and healthy fats. Staying hydrated and limiting processed sugar and caffeine can also help.
Improve Sleep Hygiene
A calm bedtime routine, limiting screen time before bed, and going to sleep at the same time each night can support deeper rest.
Manage Stress
Whether it’s deep breathing, journaling, time in nature, or talking to a friend—make space to unwind and reset.
Stay Connected
You’re not meant to do this alone. Reach out to friends, support groups, or your healthcare provider if you’re feeling isolated or unsure.
Treatment Options (Without Getting Too Technical)
If symptoms are affecting your day-to-day life, you don’t have to just put up with them. There are both hormonal and non-hormonal treatment options available. These can help with things like hot flushes, sleep issues, mood swings and more.
We’re not naming specific medications here, but we can explore your options together in a personalised, supportive consultation.
When to Reach Out for Help
It’s a good idea to speak to your doctor if:
Your periods are extremely heavy or frequent
Your mood is consistently low
You’re not sleeping despite lifestyle changes
You feel unlike yourself for more than a few weeks
Even if your symptoms seem “mild,” you deserve support and answers. Don’t wait until things feel unmanageable.
You’re Not Alone
Perimenopause is a time of transition, not decline. While it can bring challenges, it can also be a time to reconnect with your health, reassess your priorities, and build habits that support you for the long term.
If you’re wondering whether what you’re going through is “normal” or need help making sense of it all, we’re here for you.
You don’t have to figure this out on your own—book a visit or reach out to chat. We’ll meet you with empathy, good information, and support that fits your life.
A practical guide to treat Scabies
Definition – What is Scabies
Scabies is a contagious skin infestation caused by the Sarcoptes scabiei mite. It is a common and highly contagious condition that can affect people of all ages, as well as animals. Scabies mites burrow into the top layer of the skin, where they lay eggs and cause intense itching and a characteristic rash.
Common symptoms of scabies include:
Intense Itching – The most common and bothersome symptom of scabies is severe itching, which is often worse at night.
Rash – A red, pimple-like rash may develop at the site of the mite burrows. This rash can appear anywhere on the body but is most frequently found on the hands, wrists, between the fingers, elbows, armpits, breasts, buttocks, and genital area.
Blisters – In some cases, scabies can lead to the development of small, fluid-filled blisters and pustules on the skin.
Secondary Infections – Scratching the itchy rash can break the skin and lead to secondary bacterial infections.
Scabies is typically spread through close personal contact, such as shaking hands or sexual contact, but it can also be transmitted through infested bedding, clothing, or towels. It is important to note that scabies is not related to poor hygiene; anyone can get scabies.
Treatment
Since scabies is contagious, everyone in the household must be treated at the same time.
Treating scabies typically involves the use of prescription medications to kill the mites and their eggs, as well as taking steps to prevent the spread of the infestation.
Here’s a practical guide to treating scabies:
- Confirm the Diagnosis:
- Before starting treatment, it’s essential to confirm that you have scabies. Consult a healthcare professional, who can examine your skin and perform tests if necessary to diagnose scabies accurately.
2. Prescription Medications:
- Your healthcare provider will likely prescribe a scabicide medication to treat the infestation. This will depend on the age of the patient, allergies, risk factors, such as pregnancy etc.
- Commonly used scabicide options include:
- Permethrin cream 5%: This is the most common and effective treatment. It is usually applied to the entire body from the neck down. It is applied on alternative days for 2 weeks.
- Benzyl Benzoate: This is applied from the neck down everyday without bathing for 5 – 7 days.
- Ivermectin: An oral medication may be prescribed in some cases, especially for severe or resistant infestations. It is not safe in a child weighing less than 15 kgs and safety hasn’t been established in pregnant women. Depending on infection severity, ivermectin should be taken in 3 doses (Day 1, 2 & 8); 5 doses (Day 1, 2, 8, 9 & 15) or 7 doses (Day 1, 2, 8, 9, 15, 22 & 29).
- Important to note, the mites die with the oral medication or the applied creams. It is more difficult to kill the eggs, the repeated treatment is necessary to ensure that any newly hatched mites are also eliminated. Follow your healthcare provider’s instructions carerfully with regards to the timing of the creams or oral medication.
3. Application Instructions:
- Follow the specific instructions provided by your healthcare provider for the chosen scabicide. Be sure to:
- Apply the medication to clean, dry skin.
- Cover the entire body, including all folds and creases.
- Pay extra attention to the hands, feet, wrists, elbows, and genital area.
- Leave the medication on for the recommended duration before washing it off.
4. Maintain Good Hygiene:
- While undergoing treatment, maintain good hygiene practices.
- Shower or bathe daily unless using benzyl benzoate.
- Change and wash clothing and bedding regularly in hot water to prevent reinfestation. Hang in the sun or iron with a hot iron.
- Avoid sharing personal items, such as towels and clothing, with others.
5. Notify Close Contacts:
- Inform people with whom you have had close personal contact recently, as they may also need to be treated to prevent the spread of scabies.
6. Itching Management:
- While the medication works to kill the mites, you may still experience itching for several weeks. Your healthcare provider may recommend over-the-counter or prescription medications to alleviate itching.
Prevent Reinfestation:
- Follow the instructions on the treatment course that you are on. Ensure the entire household is treated together. Mix and use neem oil and tea tree oil once your treatment is complete. Apply from neck down daily for an additional 2 weeks. The tea tree oil is a natural scabicide and neem oil interrupts with the maturation of the eggs.
- Please speak to your health care professional, tea tree oil can be an irritant to the skin and must be correctly diluted with a carrier oil such as neem oil.
Be Patient:
It may take some time for the itching and rash to completely resolve after treatment. Follow your healthcare provider’s guidance and be patient during the healing process.
Remember that it’s crucial to follow your healthcare provider’s recommendations closely and complete the entire treatment regimen to ensure that scabies is fully eradicated. If you have any concerns or experience persistent symptoms, don’t hesitate to contact your healthcare provider for guidance.
Fungal Nail Infection
Fungal Nail Infection Treatment Protocol
Prescribed Antifungal Medication: [Insert Medication Name]
Important Notes:
- Fungal nail infections require consistent treatment and patience for complete resolution.
- Follow the prescribed medication regimen diligently to ensure effectiveness.
- Maintain good foot hygiene to prevent recurrence and spread of infection.
- If experiencing any adverse reactions or concerns, please contact us.
Treatment Steps:
- Medication Application:
- Wash and dry the affected nail(s) thoroughly before applying the antifungal medication.
- Apply the prescribed antifungal medication according to the provided instructions. Ensure coverage of the entire affected nail surface and the surrounding skin.
- Frequency of Application:
- Apply the medication as directed by your healthcare provider. Typically, this may range from once daily to twice daily, depending on the prescribed medication.
- Adhere strictly to the recommended frequency without skipping doses.
- Duration of Treatment:
- Continue using the antifungal medication for the full duration prescribed by your healthcare provider, even if the infection appears to improve or resolve before then.
- Fungal nail infections often require several weeks or months of treatment to eradicate completely.
- Foot Hygiene Practices:
- Keep feet clean and dry at all times. Wash feet daily with soap and water, ensuring thorough drying, especially between the toes.
- Change socks and shoes regularly, opting for breathable materials.
- Avoid walking barefoot in public areas, such as gym locker rooms or swimming pools, to prevent reinfection.
- Nail Care:
- Trim nails straight across and file down any thickened areas to reduce the surface area for fungal growth.
- Dispose of nail clippings properly to prevent spreading the infection to other nails or individuals.
- Footwear Management:
- Opt for well-ventilated shoes that allow air circulation to prevent moisture buildup.
- Consider using antifungal powders or sprays inside shoes to inhibit fungal growth.
- Follow-Up Appointments:
- Attend scheduled follow-up appointments with your healthcare provider to monitor the progress of treatment.
- Inform your healthcare provider of any challenges or changes in symptoms during follow-up visits.
Additional Recommendations:
- Maintain overall foot health by practicing good foot care habits and wearing proper footwear.
- Avoid sharing personal items such as socks, shoes, or nail clippers with others.
- If applicable, inform your healthcare provider of any underlying health conditions or medications that may impact the treatment or effectiveness of the prescribed antifungal medication.
Haemochromatosis
Haemochromatosis is a genetic disorder characterized by excessive absorption and accumulation of iron in the body. This iron overload can affect various organs and lead to a range of symptoms. It’s important to recognize these symptoms early and seek medical advice for proper diagnosis and management. Common symptoms of hemochromatosis include:
Early Symptoms:
- Fatigue and Weakness: Persistent tiredness is one of the most common early signs.
- Joint Pain: Especially in the hands and knees.
- Abdominal Pain: Discomfort in the abdominal area can occur.
- Loss of Libido and Erectile Dysfunction: Men may experience decreased sexual drive and difficulties with sexual function.
Advanced Symptoms:
- Liver Problems:
- Liver Enlargement: The liver may become swollen.
- Cirrhosis: Scarring of the liver tissue, which can lead to liver failure.
- Hepatic Cancer: Increased risk of liver cancer.
- Heart Issues:
- Cardiomyopathy: Weakening of the heart muscle.
- Arrhythmias: Irregular heartbeats.
- Heart Failure: Severe cases can lead to the heart’s inability to pump blood effectively.
- Endocrine Disorders:
- Diabetes Mellitus: Excess iron can damage the pancreas, affecting insulin production.
- Hypothyroidism: Reduced thyroid function.
- Adrenal Insufficiency: Impaired adrenal gland function.
- Skin Changes:
- Hyperpigmentation: The skin may develop a bronze or grayish hue, often referred to as “bronze diabetes.”
- Other Symptoms:
- Menstrual Irregularities: In women, heavy periods may cease.
- Depression and Mood Swings: Psychological effects can occur due to hormonal imbalances and chronic illness.
Non-Specific Symptoms:
- Numbness and Tingling: Peripheral neuropathy can cause sensations of numbness or tingling in the extremities.
- Hair Loss: Thinning hair or alopecia may occur.
When to Seek Medical Attention:
If you experience multiple symptoms listed above, especially if there’s a family history of hemochromatosis, it’s important to consult a healthcare professional. Early diagnosis and treatment can prevent or mitigate many of the serious complications associated with iron overload.
The management of hemochromatosis focuses on reducing iron levels in the body and preventing complications caused by iron overload. The main treatments and strategies include:
- Phlebotomy (Therapeutic Blood Removal)
- Primary Treatment: Regular removal of blood is the most common and effective treatment for hemochromatosis. By removing blood, iron levels in the body are reduced, as each pint of blood contains iron.
- Frequency: Initially, phlebotomies may be done once or twice a week until iron levels (measured by ferritin and transferrin saturation) reach a target range. Once levels are under control, maintenance phlebotomies may be performed every 2-4 months.
- Goal: To maintain normal iron levels and prevent organ damage.
- Chelation Therapy (When Phlebotomy is Not Possible)
- For patients who cannot tolerate phlebotomy (e.g., those with anemia), iron chelation therapy is an alternative. Drugs like deferoxamine, deferiprone, or deferasirox bind to iron and help the body eliminate it through urine or stool.
- Chelation is less common but is useful in specific cases, such as in those with other blood disorders.
- Dietary Modifications
- Avoid Iron-Rich Foods: Reduce the intake of iron-rich foods like red meat, liver, and iron-fortified foods.
- Limit Vitamin C: Vitamin C increases iron absorption, so it is advisable to avoid excessive supplements.
- Avoid Raw Shellfish: People with hemochromatosis are at higher risk of infection from Vibrio vulnificus, a bacterium found in raw shellfish.
- Avoid Alcohol: Alcohol can damage the liver, and people with hemochromatosis are already at increased risk of liver issues.
- Monitoring Iron Levels
- Regular blood tests are needed to monitor ferritin levels and transferrin saturation to ensure that iron levels stay within a healthy range.
- Liver Function Tests: Since the liver is often affected, regular liver function tests and ultrasounds may be performed to monitor for complications like cirrhosis or liver cancer.
- Managing Complications
- Liver Disease: Patients with cirrhosis should be screened regularly for liver cancer with imaging (e.g., ultrasound) and alpha-fetoprotein (AFP) blood tests.
- Diabetes Management: Blood sugar levels should be monitored if the pancreas is affected.
- Heart Disease: Patients with cardiomyopathy or arrhythmias may need heart function monitoring and specific treatments.
- Hormonal Therapy: If iron overload affects hormone-producing glands (like the thyroid or pituitary), hormone replacement therapy may be necessary.
- Genetic Counseling
- Hemochromatosis is a hereditary condition, so family members of affected individuals should consider genetic testing and screening to detect early signs of iron overload, particularly first-degree relatives (siblings, children).
- Regular Follow-Up
- Long-term follow-up care with a healthcare provider is essential. This includes regular assessments for symptoms of iron overload and potential complications, especially in organs like the liver, heart, and endocrine glands.
- Lifestyle Considerations
- Regular Exercise: Moderate exercise is encouraged to maintain overall health and well-being.
- Hydration: Staying hydrated is important, especially when undergoing phlebotomy, as blood removal can cause dehydration.
With timely treatment, individuals with hemochromatosis can manage their condition well and prevent serious complications. Early detection and consistent monitoring are key to successful management.
Managing Hypertension
Managing hypertension effectively often involves the use of various classes of medications, each working through different mechanisms to lower blood pressure. Below is a comprehensive list of common antihypertensive medications categorized by their classes, along with their typical side effects. It’s important to remember that individual responses to medications can vary, and not everyone will experience all listed side effects. Always consult with a healthcare professional before starting or changing any medication regimen.
1. Thiazide Diuretics
Examples:
- Hydrochlorothiazide (HCTZ)
- Chlorthalidone
- Indapamide
Mechanism of Action: Thiazide diuretics help the kidneys eliminate sodium and water, reducing blood volume and decreasing vascular resistance.
Common Side Effects:
- Increased urination
- Electrolyte imbalances (e.g., low potassium [hypokalemia], low sodium [hyponatremia], low magnesium)
- Elevated blood sugar levels
- Elevated cholesterol and triglyceride levels
- Dizziness or lightheadedness, especially upon standing (orthostatic hypotension)
Less Common Side Effects:
- Gout attacks
- Photosensitivity (skin sensitivity to sunlight)
- Muscle cramps
2. Calcium Channel Blockers (CCBs)
Examples:
- Amlodipine
- Diltiazem
- Verapamil
- Felodipine
Mechanism of Action: CCBs prevent calcium from entering heart and blood vessel muscle cells, resulting in relaxed and widened blood vessels, which lowers blood pressure.
Common Side Effects:
- Swelling of the ankles and feet (peripheral edema)
- Flushing
- Dizziness
- Headache
- Palpitations (awareness of heartbeats)
Less Common Side Effects:
- Constipation (more common with verapamil)
- Fatigue
- Nausea
3. Angiotensin-Converting Enzyme Inhibitors (ACE Inhibitors)
Examples:
- Lisinopril
- Enalapril
- Ramipril
- Benazepril
Mechanism of Action: ACE inhibitors block the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor, leading to relaxed blood vessels and lower blood pressure.
Common Side Effects:
- Persistent dry cough
- Elevated blood potassium levels (hyperkalemia)
- Low blood pressure (hypotension)
- Dizziness
- Fatigue
Less Common Side Effects:
- Kidney dysfunction
- Angioedema (swelling of deeper layers of the skin, often around the eyes and lips)
- Increased blood urea nitrogen (BUN) and serum creatinine
Important Note: ACE inhibitors are generally not recommended during pregnancy due to the risk of fetal injury or death.
4. Angiotensin II Receptor Blockers (ARBs)
Examples:
- Losartan
- Valsartan
- Olmesartan
- Irbesartan
Mechanism of Action: ARBs block angiotensin II from binding to its receptors on blood vessels, preventing vasoconstriction and lowering blood pressure.
Common Side Effects:
- Dizziness
- Elevated blood potassium levels (hyperkalemia)
- Fatigue
- Headache
Less Common Side Effects:
- Kidney dysfunction
- Diarrhea
- Nasal congestion
Advantages Over ACE Inhibitors: ARBs typically do not cause the persistent dry cough associated with ACE inhibitors and have a lower risk of angioedema.
5. Beta-Blockers
Examples:
- Metoprolol
- Atenolol
- Propranolol
- Bisoprolol
- Carvedilol
Mechanism of Action: Beta-blockers reduce the heart rate and the force of contraction, which decreases the amount of blood pumped by the heart and lowers blood pressure.
Common Side Effects:
- Fatigue
- Cold hands and feet
- Weight gain
- Depression
- Bradycardia (slow heart rate)
Less Common Side Effects:
- Shortness of breath (especially in those with asthma)
- Sexual dysfunction
- Sleep disturbances or nightmares
Important Considerations: Beta-blockers are particularly useful in patients with certain conditions such as ischemic heart disease, heart failure, or after a heart attack. They are generally not first-line therapy for hypertension without these additional indications.
6. Alpha-Blockers
Examples:
- Doxazosin
- Prazosin
- Terazosin
Mechanism of Action: Alpha-blockers relax certain muscles and help small blood vessels remain open, reducing blood pressure.
Common Side Effects:
- Dizziness or lightheadedness, especially upon standing (orthostatic hypotension)
- Headache
- Pounding heartbeat (palpitations)
- Weakness
Less Common Side Effects:
- Nasal congestion
- Nausea
- Fatigue
Primary Use: Often used to treat symptoms of benign prostatic hyperplasia (BPH) in addition to managing hypertension.
7. Centrally Acting Agents
Examples:
- Clonidine
- Methyldopa
- Reserpine
Mechanism of Action: These medications work in the brain to decrease nerve signals that narrow blood vessels, leading to lowered blood pressure.
Common Side Effects:
- Drowsiness or sedation
- Dry mouth
- Constipation
- Fatigue
- Dizziness
Less Common Side Effects:
- Rebound hypertension if the medication is abruptly stopped
- Depression (especially with reserpine)
Important Considerations: Centrally acting agents are typically reserved for resistant hypertension or specific clinical scenarios due to their side effect profiles.
8. Direct Vasodilators
Examples:
- Hydralazine
- Minoxidil
Mechanism of Action: Direct vasodilators relax the muscles in blood vessel walls, leading to widened arteries and reduced blood pressure.
Common Side Effects:
- Headache
- Tachycardia (rapid heart rate)
- Fluid retention, which may require the use of diuretics
- Pericardial effusion (rare, especially with hydralazine)
Less Common Side Effects:
- Lupus-like symptoms (more common with hydralazine)
- Excessive hair growth (with minoxidil, primarily used topically for hair loss)
Important Considerations: Direct vasodilators are often used in severe or refractory hypertension and typically require combination with other antihypertensive agents to mitigate side effects like reflex tachycardia.
9. Renin Inhibitors
Examples:
- Aliskiren
Mechanism of Action: Renin inhibitors block the enzyme renin, which plays a key role in the renin-angiotensin-aldosterone system (RAAS), leading to decreased production of angiotensin I and II, and thus lowering blood pressure.
Common Side Effects:
- Diarrhea
- Dizziness
- Fatigue
- Headache
Less Common Side Effects:
- Elevated blood potassium levels (hyperkalemia)
- Kidney dysfunction
Important Considerations: Renin inhibitors are a newer class of antihypertensives and are typically considered when other RAAS inhibitors (ACE inhibitors or ARBs) are not suitable.
10. Aldosterone Antagonists
Examples:
- Spironolactone
- Eplerenone
Mechanism of Action: These medications block the effects of aldosterone, a hormone that causes the kidneys to retain sodium and water, thereby reducing blood volume and lowering blood pressure.
Common Side Effects:
- Elevated blood potassium levels (hyperkalemia)
- Gynecomastia (particularly with spironolactone)
- Menstrual irregularities (with spironolactone)
- Fatigue
Less Common Side Effects:
- Gastrointestinal disturbances
- Dizziness
Important Considerations: Aldosterone antagonists are often used in patients with resistant hypertension or specific conditions like heart failure or certain forms of kidney disease.
11. Combination Medications
Examples:
- Amlodipine/Benazepril (Lotrel)
- Lisinopril/Hydrochlorothiazide (Zestoretic)
- Olmesartan/Amlodipine (Azor)
Mechanism of Action: These medications combine two antihypertensive agents from different classes to enhance blood pressure-lowering effects and improve patient adherence by reducing the number of pills needed.
Common Side Effects:
- Varies depending on the combination, but may include dizziness, cough (from ACE inhibitors), swelling (from calcium channel blockers), and electrolyte imbalances.
Less Common Side Effects:
- Increased risk of side effects from both component medications.
Important Considerations: Combination therapies can be more effective than monotherapy in achieving target blood pressure levels and are often used when a single medication does not adequately control hypertension.
12. Beta-Blocker and Diuretic Combinations
Examples:
- Bisoprolol/Hydrochlorothiazide (Ziac)
- Metoprolol/Hydrochlorothiazide (Lopressor HCTZ)
Mechanism of Action: Combining a beta-blocker with a diuretic leverages the complementary mechanisms to better control blood pressure.
Common Side Effects:
- Side effects associated with both beta-blockers and diuretics, such as fatigue, dizziness, electrolyte imbalances, and increased urination.
Less Common Side Effects:
- Increased risk of side effects from both components, including bradycardia and hypotension.
Important Considerations: These combinations are useful for patients requiring multiple mechanisms to manage their hypertension effectively.
General Considerations for Antihypertensive Medications
Individual Variability:
- Responses to antihypertensive medications can vary based on genetics, age, race, underlying health conditions, and other factors. What works well for one person may not be as effective or may cause undesirable side effects in another.
Comorbid Conditions:
- The presence of other health issues (e.g., diabetes, kidney disease, heart disease) can influence the choice of antihypertensive medication. For example, ACE inhibitors or ARBs are often preferred in patients with diabetes or chronic kidney disease.
Side Effect Management:
- Monitoring and managing side effects is crucial. If side effects are severe or persistent, it’s important to consult a healthcare provider, who may adjust the dosage or switch to a different medication.
Lifestyle Modifications:
- Medications are most effective when combined with lifestyle changes such as a balanced diet (e.g., DASH diet), regular physical activity, weight management, limiting alcohol intake, and avoiding tobacco use.
Adherence to Medication:
- Consistently taking medications as prescribed is essential for effective blood pressure control. Missing doses can lead to uncontrolled hypertension and increased risk of complications.
Regular Monitoring:
- Regular blood pressure monitoring and follow-up appointments with a healthcare provider help ensure that the chosen medication regimen is effective and allows for timely adjustments if needed.
Final Recommendations
Consult a Healthcare Professional: Always seek personalized medical advice from a healthcare provider before starting, stopping, or changing any medication. They can tailor the treatment plan based on your specific health needs and circumstances.
Report Side Effects: Inform your healthcare provider about any side effects you experience. They can help manage these effects, whether by adjusting the dosage or switching to a different medication.
Medication Interactions: Be aware of potential interactions between antihypertensive medications and other drugs or supplements you may be taking. Always discuss your complete medication list with your healthcare provider.
Do Not Self-Medicate: Avoid adjusting your medication regimen without professional guidance, as improper use can lead to serious health risks.
Managing hypertension is a multifaceted process that often requires a combination of medication, lifestyle changes, and regular medical supervision. By understanding the various antihypertensive options and their potential side effects, you can work collaboratively with your healthcare provider to achieve optimal blood pressure control and reduce the risk of complications.
The Importance of Weight Loss for Hypertensive Patients
Hypertension, or high blood pressure, is a common and serious condition that affects millions of people worldwide. It is often referred to as the “silent killer” because it can go unnoticed for years while causing damage to vital organs, including the heart, kidneys, and brain. One of the most impactful lifestyle changes for managing and even preventing high blood pressure is weight loss.
How Weight Affects Blood Pressure
Excess body weight contributes to hypertension through multiple mechanisms. Carrying extra pounds places additional strain on the heart, requiring it to pump harder to circulate blood throughout the body. This increased workload raises blood pressure. Fat tissue, especially visceral fat around the abdomen, can also release hormones and inflammatory chemicals that negatively affect blood vessel function and promote hypertension.
Moreover, being overweight is often associated with other conditions that elevate blood pressure, such as insulin resistance, sleep apnea, and an unhealthy lipid profile. Losing weight helps address these underlying issues, contributing to better blood pressure control.
The Benefits of Weight Loss for Hypertensive Patients
Lowering Blood Pressure: Even modest weight loss can have a significant impact on blood pressure levels. Studies show that losing just 5-10% of body weight can lower systolic and diastolic blood pressure, improving overall cardiovascular health.
Reducing the Need for Medication: For many people, weight loss can reduce the need for antihypertensive medication or, in some cases, even eliminate it altogether. This not only saves on healthcare costs but also minimizes the risk of medication-related side effects, including fatigue, dizziness, and sexual dysfunction.
Improving Heart Health: Weight loss can lead to a reduction in LDL cholesterol (“bad” cholesterol) and triglycerides while increasing HDL cholesterol (“good” cholesterol). These changes promote heart health, reducing the risk of heart attacks and strokes, which are more common in people with high blood pressure.
Enhancing Vascular Function: Excess weight can cause blood vessels to become stiffer and less elastic. Weight loss helps restore proper blood vessel function, making it easier for blood to flow and reducing the pressure exerted on artery walls.
Alleviating Sleep Apnea: Many overweight or obese individuals suffer from sleep apnea, a condition that can worsen hypertension. Weight loss has been shown to reduce the severity of sleep apnea, resulting in better sleep and improved blood pressure control.
Conclusion
Weight loss is a powerful tool in the fight against hypertension. By reducing excess weight, patients can experience dramatic improvements in blood pressure, heart health, and overall well-being. While the journey may be challenging, the long-term rewards—including a lower risk of cardiovascular disease and greater energy—make it a vital step toward a healthier, more vibrant life.
If you’re struggling with weight management or need guidance tailored to your health conditions, don’t hesitate to reach out to our healthcare professionals who can support your journey to better blood pressure and overall health.
Inflamed Sphincter
Constipation can lead to a variety of complications, including inflammation in different parts of the pelvic area. Here’s how constipation can potentially contribute to the issues you’re asking about:
- Inflamed Sphincter (Anal Sphincter)
- Cause: When someone is constipated, they may strain excessively during bowel movements. This can put a lot of pressure on the anal sphincter, leading to muscle irritation or inflammation. In severe cases, this may also cause small tears or fissures, which can further aggravate the area.
- Symptoms:
- Painful bowel movements
- Anal itching or discomfort
- Possible bleeding from small tears (anal fissures)
- Link Between Constipation and Prostate Inflammation
- Prostatitis (inflammation of the prostate) can be indirectly related to chronic constipation. Here’s how:
- Pressure on the Prostate: The rectum is located near the prostate gland. Chronic constipation can cause the rectum to become distended, which can exert pressure on the prostate, leading to discomfort or inflammation.
- Urinary Issues: Constipation can also press on the bladder or the urethra, leading to urinary retention or frequent urges to urinate, which may aggravate prostate issues.
- Chronic Inflammation: In some cases, straining and pressure from constipation can cause chronic pelvic pain, which may be mistaken for prostatitis or exacerbate existing prostate conditions.
- Managing Constipation to Reduce Inflammation
- Dietary Changes: Increasing fiber intake (fruits, vegetables, whole grains) and staying hydrated can help soften stool and reduce straining.
- Regular Exercise: Helps maintain regular bowel movements and can reduce pelvic pressure.
- Stool Softeners: For chronic cases, stool softeners or laxatives might be needed, but these should only be used as per medical advice.
- Pelvic Floor Exercises: Strengthening the pelvic floor may help in relieving tension on both the sphincter and the prostate.
Patients have stopped statins due to fear of side effects. Much of this fear comes from stories online or from friends, rather than from medical facts. While side effects can occur, statins remain one of the most effective medicines for protecting the heart.
Why Are People Afraid of Statins?
The most common concerns patients report are:
- Muscle aches or cramps
- Tiredness or fatigue
- Mild memory or concentration problems
- Raised liver enzymes on blood tests
- Slight increase in blood sugar in some people
Most people do not experience serious side effects. When side effects do occur, they are often mild, dose-related, and reversible. Many patients tolerate a different statin or a lower dose very well.
Why Taking a Statin Can Save Your Life
Statins do more than just lower cholesterol:
- Lower “bad” LDL cholesterol
- Reduce inflammation in blood vessels
- Stabilise cholesterol plaques (making them less likely to rupture)
- Reduce the risk of heart attacks and strokes
- Improve long-term survival
For patients with heart disease, diabetes, or very high cholesterol, statins are proven to reduce death and serious heart events.
Older vs Newer Statins
Not all statins are the same.
Older statins (e.g. Simvastatin):
- Less powerful cholesterol lowering
- More interactions with other medicines
- Higher chance of muscle side effects at higher doses
Newer statins (e.g. Atorvastatin [Aspavor] and Rosuvastatin [Crestor]):
- Stronger cholesterol-lowering effect
- Work well at lower doses
- Fewer drug interactions
- Generally better tolerated
Many patients who struggle with simvastatin do very well on newer statins.
If You Do Not Want to Take a Statin
Some patients cannot tolerate statins or choose not to take them. In low-risk patients, natural cholesterol products may be considered with medical guidance.
Common Ingredients in Natural Cholesterol Balance Products:
- Plant sterols/stanols – reduce cholesterol absorption in the gut
- Bergamot extract – helps lower LDL cholesterol
- Berberine – improves cholesterol and blood sugar control
- Soluble fibre (psyllium, beta-glucans) – binds cholesterol in the intestine
- Omega-3 fatty acids – reduce triglycerides and inflammation
- Artichoke extract – supports liver and cholesterol metabolism
⚠️ Some products contain red yeast rice, which acts like a natural statin and can have similar side effects.
When Natural Products Are NOT Safe or Enough
Natural products should not be used alone if you have:
- Very high or extreme cholesterol levels
- A previous heart attack, stroke, stent, or bypass surgery
- Poor metabolic health, including:
- Diabetes
- Insulin resistance
- Metabolic syndrome
- Central obesity or fatty liver
In these situations, natural products do not lower cholesterol enough and do not protect the heart the way statins do. Relying on them can give a false sense of safety while heart disease silently worsens.
The Bottom Line
Statins are not dangerous for most people and are life-saving for high-risk patients. Fear should never replace facts. If side effects occur, changing the type or dose of statin often solves the problem. Natural products may help some people, but they are not a replacement for statins in high-risk patients.
Always speak to your doctor before stopping your statin—your heart health depends on it.
Eczema on the Hands
Medical Treatment
1. Topical Medications
- During the day Application:
- Apply a thin layer of topical ointment as directed to affected areas.
- Morning and Evening Application:
- Mix topical ointment with 40g emollient cream in equal parts and apply to the affected areas.
2. Emollients
- Use a thick, fragrance-free emollient (e.g., Epi-max, Cetaphil, or CeraVe) liberally throughout the day to keep the skin hydrated.
- Reapply emollients after washing hands or exposure to water.
Practical Tips for Symptom Management
1. Protect the Skin
- Cotton Gloves at Night:
- After applying the evening mixture of topical ointment and emollient cream, wear cotton gloves to enhance absorption and prevent scratching during sleep.
- Protective Gloves During Daytime:
- Use nitrile gloves when doing household chores, like washing dishes, to avoid irritants and water exposure.
- Avoid latex gloves, as they may trigger irritation or allergic reactions.
2. Avoid Triggers
- Minimize contact with known irritants, such as:
- Harsh soaps, detergents, and cleaning chemicals.
- Prolonged exposure to water.
- Choose mild, hypoallergenic hand soaps or cleansers – CeraVe face wash
3. Manage Sweat
- Keep hands and feet dry, as excessive sweating can exacerbate eczema.
- Use a fan or moisture-absorbing powder to reduce sweating in the affected areas.
4. Reduce Itching
- Apply a cold compress to reduce itchiness and inflammation.
- Take oral antihistamines (e.g., loratadine or cetirizine) at bedtime to help manage itching and improve sleep.
Long-Term Care
1. Maintenance Treatment
- Continue using emollients daily, even during periods of remission, to maintain the skin barrier.
- Once active inflammation subsides, reduce steroid application frequency to twice or three times per week to prevent flares.
2. Address Secondary Infections
- If signs of infection (e.g., oozing, crusting, or increased redness) develop, consult a healthcare provider.
Lifestyle Adjustments
- Moisturize after bathing: Pat skin dry and apply emollient within 3 minutes to lock in moisture.
- Avoid extreme temperatures: Protect skin from excessive heat or cold, which can worsen symptoms.
Lymphaderma
You have a condition known as lymphedema, which refers to swelling that occurs when the lymphatic system is not able to properly drain lymph fluid. This fluid builds up in the tissues, most commonly in the arms or legs, although other areas can be affected depending on the cause.
The lymphatic system is part of your immune system and is responsible for circulating lymph — a clear fluid containing white blood cells, proteins, and waste products — throughout the body. When the lymphatic vessels or lymph nodes are damaged or blocked, fluid can accumulate, leading to the swelling you’re experiencing.
Lymphedema can be classified as either primary (due to a congenital or inherited abnormality in the lymphatic system) or secondary, which is more common and often occurs after surgery, radiation, infection, trauma, or cancer treatment.
Although lymphedema is a chronic condition, it can be effectively managed. Treatment typically includes compression therapy, manual lymphatic drainage (a specialized form of massage), exercise, skin care to prevent infection, and in some cases, surgical intervention. The goal is to reduce the swelling, improve function, and prevent complications such as infections or fibrosis.
We’ll work together to create a long-term management plan tailored to your needs, and I may also refer you to a lymphedema therapist for specialized care.
Practical Tips for Symptom Management
1. Compression Therapy
Wear compression garments (sleeves, stockings, or wraps) as advised. These help move fluid out of the affected limb.
Put them on first thing in the morning before swelling increases.
Make sure they fit properly — too loose won’t help; too tight can worsen the condition.
Replace garments every 4–6 months or as needed.
2. Manual Lymphatic Drainage (MLD)
See a certified lymphedema therapist for lymphatic massage.
They can also teach you self-massage techniques to do at home.
Daily self-MLD can be helpful for maintenance, especially in early stages.
3. Exercise and Movement
Do gentle, regular exercise such as walking, swimming, stretching, or light strength training.
Movement helps stimulate lymph flow.
Avoid high-impact or very strenuous exercise unless cleared by a healthcare provider.
4. Elevate the Affected Limb
When resting, elevate the limb above the level of the heart when possible.
Use pillows to support the arm or leg, especially while sleeping or sitting for long periods.
5. Skin Care & Hygiene
Keep the skin clean and moisturized to prevent cracks or dryness.
Avoid cuts, insect bites, and burns — even small injuries can lead to infection (cellulitis).
Treat any wounds promptly and report signs of infection (redness, heat, fever) immediately.
6. Avoid Heat and Constriction
Avoid hot tubs, saunas, or prolonged heat exposure — heat increases swelling.
Don’t wear tight clothing or jewelry on the affected limb.
Avoid blood pressure cuffs or needle sticks on the affected side if possible.
7. Weight Management
Maintaining a healthy body weight can reduce strain on the lymphatic system.
Diet rich in fruits, vegetables, whole grains, and lean protein can support tissue health.
8. Travel Precautions
When flying or sitting for long periods:
- Wear compression garments.
- Walk or move around regularly.
- Stay hydrated.
Potential Benefits of Laser Therapy for Lymphedema
Clinical studies and practice suggest that LightForce laser therapy may help:
1. Reduce Limb Swelling
Can modestly reduce the volume of the affected limb, especially in early or moderate lymphedema.
2. Enhance Lymphatic Flow
May stimulate the lymph vessels and promote better drainage of lymph fluid.
3. Soften Fibrotic Tissue
Helpful in managing skin thickening and fibrosis, particularly in chronic lymphedema.
4. Relieve Pain and Discomfort
Has anti-inflammatory effects and may reduce pain, stiffness, and pressure in the affected limb.
5. Support Tissue Healing
May assist in regenerating damaged lymphatic structures and preventing complications such as cellulitis.
⚠️ Important Consideration
🔹 Adjunctive Therapy
Laser therapy should be viewed as a supportive treatment, not a standalone solution. It works best when used alongside standard lymphedema care, including compression therapy, manual lymphatic drainage (MLD), prescribed exercise, and skin care.